ARTESp (Acute Recanalization of Thrombo-Embolic Ischemic Stroke with pREset®) is a prospective, multicenter, single-arm Post Market Clinical Follow-up study in which the efficacy, the safety and the long-term outcomes of mechanical thrombectomy using the pREset® Thrombectomy Device were evaluated. The study included patients with acute proximal occlusions of major cerebral vessels of both the anterior and posterior circulation.
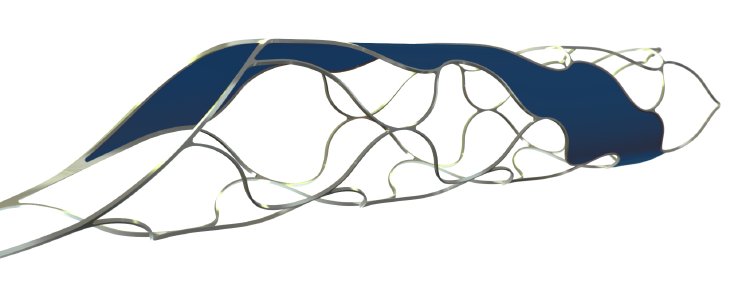
Such cerebral occlusions are the main cause of ischemic strokes resulting in permanent disability and the second cause of death in the western world. Thrombectomy systems like the pREset® enable the treating physicians to quickly restore blood flow in the patient’s brain, by removing the clot from the artery.
Overall, 100 patients with 109 acute intracranial vessel occlusions were included in the ARTESp study. The average age of the patients was 68.3 years and they presented with a mean NIHSS5 of 15. The rate of vessel recanalization (re-opening) (TICI6 2b/3) was 84.4%. After 90 days, 62.5% of the patients had a positive clinical outcome and were free of severe, neurological deficits (modified Rankin Scale mRS 0-2). The mortality rate was 7%.
“Considering the increased evidence in favor of mechanical thrombectomy and the outstanding results of ARTESp, it is vitally important that the pREset® Thrombectomy Device is available for doctors who treat patients with ischemic stroke,” says Dr. Hermann Monstadt, Managing Partner, phenox GmbH. “In the interest of adding clinical evidence for thrombectomy we are delighted that the pREset® and pREset® LITE Thrombectomy Devices are now included, among others, in the SITS Open study.” The SITS Open study under the direction of the neuroscientific department at Karolinska Institute, Sweden, strives to compare the stand-alone use of intravenous clot busting drugs to mechanical thrombectomy. This study hopes to add further evidence for the use of mechanical thrombectomy as a first line and standard of care treatment for proximal large vessel occlusion ischemic strokes.
The results of the ARTESp study were published in the following paper:
Prothmann et al.; Acute Recanalization of Thrombo-Embolic Ischemic Stroke with pREset (ARTESp): the impact of occlusion time on clinical outcome of directly admitted and transferred patients; J NeuroIntervent Surg 2016; doi:10.1136/neurintsurg-2016-012556.
Further references:
1Berkhemer et al.; A Randomized Trial of Intraarterial Treatment for Acute Ischemic Stroke; N Engl J Med 2014; DOI: 10.1056/NEJMoa1411587.
2Saver et al.; Stent-Retriever Thrombectomy after Intravenous t-PA vs. t-PA Alone in Stroke; N Engl J Med 2015; DOI: 10.1056/NEJMoa1415061.
3Campbell et al.; Endovascular Therapy for Ischemic Stroke with Perfusion-Imaging Selection; N Engl J Med 2015; DOI: 10.1056/NEJMoa1414792.
4Goyal et al.; Randomized Assessment of Rapid Endovascular Treatment of Ischemic Stroke; N Engl J Med 2015; DOI: 10.1056/NEJMoa1414905.
5NIHSS = NIH Stroke Scale
6TICI = Thrombolysis in Cerebral Infarction